From Paper to Pixels: Developing an EHR Powered by FHIR
Understanding EHR Systems
An electronic health record (EHR) system is a digital version of a patient’s paper chart. EHRs can store patient information, medical images, lab results, and other clinical data.
Why Electronic Health Records (EHRs) Matter:

Traditional way
The traditional paper-based approach not only leads to difficulties in managing records but also burdens patients with the responsibility of safeguarding and organizing their X-ray reports and other medical documents, which can be overwhelming and prone to loss or damage. Transitioning to electronic health records (EHRs) addresses these challenges by providing patients with secure digital access to their medical records, ensuring convenience, reliability, and peace of mind in managing their healthcare information.
FHIR Basics and Relation to EHR:
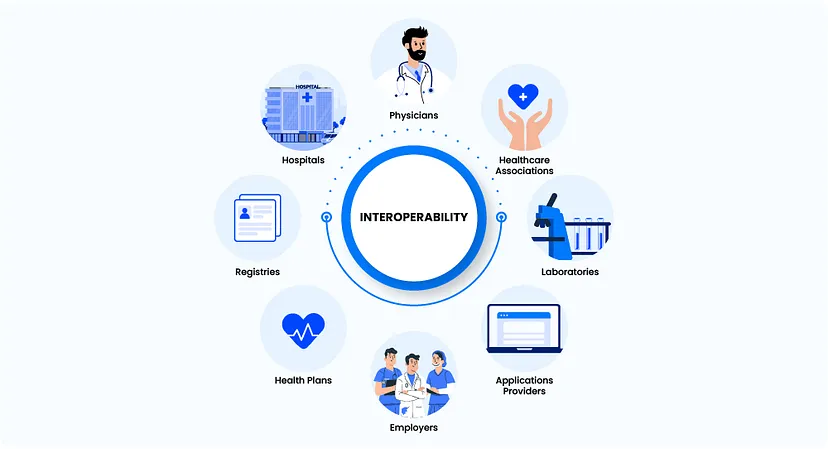
FHIR, a standard for electronically exchanging healthcare data, offers a modular and standardized framework for interoperability. Acting as a bridge for EHR systems, FHIR enables seamless data exchange, integration across platforms, and improved patient care.
Here’s a simple example of how FHIR works:

- 1. Meet Sara: Meet Sarah. She’s been seeing Dr. Smith for years for her regular check-ups.
- 2. Recentl: Sarah moved to a new city and needs to find a new doctor.
- 3. Appointment with Dr. Johnson: She schedules an appointment with Dr. Johnson, a specialist recommended by a friend.
- 4. FHIR in Action: Instead of worrying about transferring her medical records manually, Sarah’s old clinic uses FHIR to securely share her medical history, prescriptions, and test results with Dr. Johnson’s office.
- 5. Seamless Transition: During her first visit with Dr. Johnson, he already knows about her allergies, past surgeries, and current medications, making the transition seamless for Sarah and ensuring she receives the best possible care from the start.
Building an EHR with FHIR:
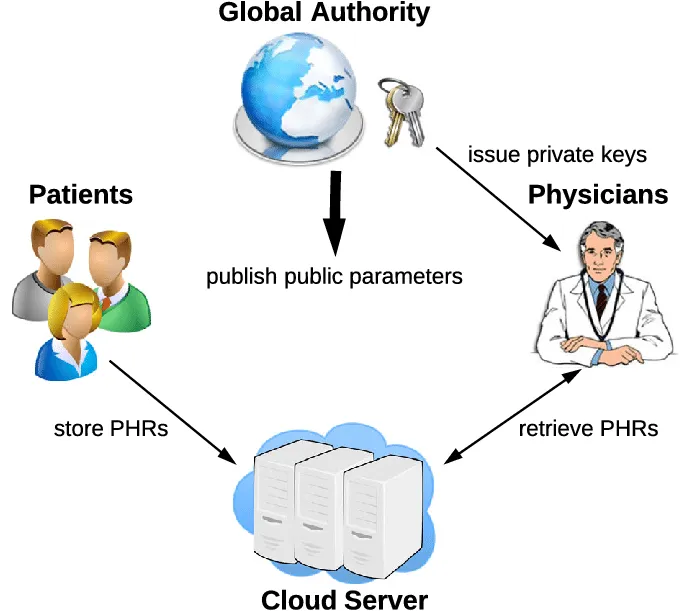
Building an EHR with FHIR involves setting up a FHIR server for data storage and adopting the standard’s modular framework to map patient data. Implementation of CRUD operations via FHIR RESTful APIs enables seamless interaction with patient records. Security measures like authentication and encryption ensure compliance with regulations like HIPAA. Rigorous testing validates functionality, while comprehensive documentation aids developers and healthcare professionals, ultimately optimizing workflows and improving patient care.
Conclusion:
In conclusion, the transition from traditional paper-based health records to Electronic Health Records (EHRs) powered by FHIR standards emerges as a pivotal advancement in healthcare data management. This shift not only addresses the challenges of manual record-keeping and patient burden but also fosters a more efficient and secure system.
Discover more blogs on healthcare and technology at Tacten